Osteoporosis is an invisible disease – until you have a fracture. We don’t see our bones breaking down over time.

“Men and women both start losing bone early in life, but we don’t see the consequences until later in life,” said Nahid J. Rianon, MD, a geriatrician with UT Physicians Center for Healthy Aging – Bellaire Station.
Osteoporosis starts showing changes in the trabecular bone, which is why bone density tests are performed in the spine and the hip area, where more of it exists. The general recommendation is to begin bone density testing at age 65 for women and 70 for men. Other factors can dictate earlier testing.
New technology provides more precision
Trabecular bone score (TBS) can provide a more accurate assessment of bone health through technology, specifically for patients with diabetes or those taking certain medications long term. Software is added to bone density machines that can detect structural deterioration and predict new fractures. At UT Physicians, the team adds TBS to the traditional bone density score to get a better picture of an older individual’s bone health. Currently, TBS is available in the UT Physicians Internal Medicine – Texas Medical Center clinic.
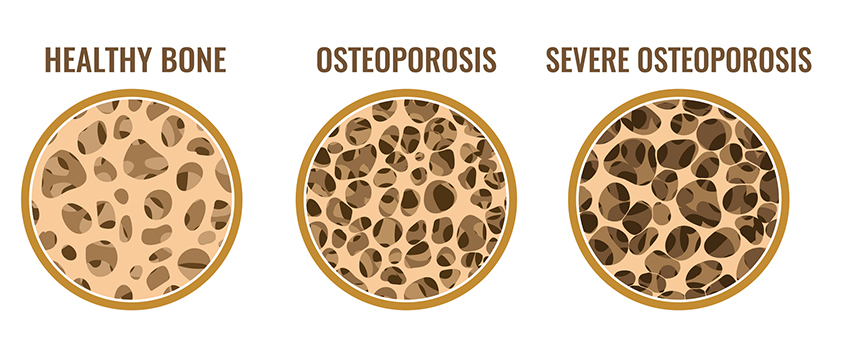
Rianon, professor and Memorial Hermann Chair in geriatrics at McGovern Medical School at UTHealth Houston, compared bones to a building as an example of structural deterioration. The bones develop holes with osteoporosis as the columns break down and become structurally weak. Heavy pressure crushes it, and bones can’t hold the weight anymore.
Broken bones from osteoporosis
Rianon frequently sees patients who have broken a bone, but whose bone density tests don’t indicate osteoporosis. This illustrates the value of the trabecular bone score.
“We want to know this so we can help certain patients who haven’t shown that change in bone density yet,” Rianon said. “With TBS, we can discover their poor bone quality and start treatment to prevent a future fracture. This knowledge impacts my treatment plan and patients’ future potential to maintain their independence.”
Rianon cautioned that shrinking more than 2.5 inches in height could be an indicator of a vertebral fracture due to structural deterioration. Only one-third of patients experience pain from a vertebral fracture, so they may not even know.
Fracture Risk Assessment Tool (FRAX) is an online tool developed by the World Health Organization that estimates your risk for osteoporosis. The algorithms provide a 10-year probability of hip fracture and a 10-year probability of a major osteoporotic fracture. The tool is intended for people 40-90 years old.
Eating for strong bones
It’s never too early to start prepping for strong bones. Bone loss happens to everyone, said Rianon.
“Women just start losing more during menopause due to estrogen deficiency,” she said.
Individuals accrue bone as they grow and reach peak bone mass between their 20s and 30s. Bone loss starts after one reaches the peak bone mass. Nutrition plays a role from early in life well into later years regarding bone health.
Rianon said if we don’t grow up with good nutrition, we aren’t accruing good bone health to reach our peak. As a result, we start losing bone mass from a lower level. If individuals don’t have good nutrition later in life, they can’t maintain what they have.
Nutrition is described as everything that builds our bodies, including protein, carbohydrates, and fat. In the clinical world, providers look at vitamin D and calcium levels. Medications for treating osteoporosis won’t work appropriately if vitamin D is not on target. Calcium levels in the blood that move up and down could be a sign that something else is wrong.
“We need to make sure there aren’t underlying health conditions causing abnormal calcium and vitamin D levels,” Rianon said. “It goes beyond ‘Do you have enough vitamin D and calcium?’ For example, there could be problems relating to kidneys or the parathyroid hormone gland.”
Choosing appropriate medicine
Medications are available for osteoporosis, ranging from those that slow the progression of bone deterioration to new ones that help form bone. As we age, bones break down faster than formation can keep up. Resorption is the breakdown of bone.
Rianon said medications have protocols for their duration of use. Some can be used long term with an intermittent pause, known as a drug holiday. Others have limited lifetime durations of one to two years. When these medications aren’t used in accordance with the appropriate protocols, the bone structure can change at the cellular level and increase the risk of a different kind of fracture. Rianon emphasized the importance of talking to your doctor and discussing which medication is appropriate and for how long, according to your medical profile.


