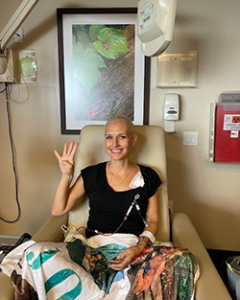
When Jennifer Setterbo of Cypress learned she had breast cancer, it was the beginning of a personal health journey, as well as courage in seeking care and advice essential to her treatment and a cure. It is an inspiring story of perseverance and resilience.
Jennifer’s gynecologist recommended a mammogram during her annual exam in August 2020 based on a family history of breast cancer, but she elected to follow up at a later date. In April 2021, Jennifer discovered a lump in her right breast during a self-exam after receiving a COVID-19 shot.
The results of Jennifer’s mammogram came back negative. She was advised it may be a swollen lymph node from the COVID-19 shot, but the lump showed no signs of subsiding after several weeks.
“I went again to get the lump checked, and the nurse practitioner used the word worrisome, which I knew wasn’t good,” Jennifer said.
By the start of 2022, Jennifer would learn she had a case of stage 2 case breast cancer. In addition, she discovered she had very dense breast tissue, which made it important to undergo thorough examinations and be fully apprised of her condition.
Steps to treatment
Soon after the diagnosis, genetic testing revealed Jennifer had a BRCA2 gene mutation, which increased the risk of other cancers forming. She also received an Oncotype DX test to determine if chemotherapy would aid in cancer treatment.
“Based on the Oncotype DX test results, the doctors gave an opinion that chemotherapy would not be effective for my treatment,” Jennifer said. “As a first step, they recommended I have my ovaries and fallopian tubes removed, based on the BRCA2 finding.”
Following the ovary and fallopian tube removal procedure, doctors recommended hormone therapy to reduce the size of identified tumors.

Next, Jennifer met with Jessica Treviño Jones, MD, an oncologist with UT Physicians.
“In reviewing Jennifer’s case, we noted there was new information and data on breast cancer in the last six months that we felt should be factored into her treatment,” said Jones, who is an assistant professor with McGovern Medical School at UTHealth Houston. “The form of cancer for which Jennifer was diagnosed normally occurs in older women and responds to hormonal therapy. In this case of an estrogen-positive breast cancer, a strategy for treatment was needed that was more aggressive and would aid in treating her lymph nodes, which had been affected.”
Jennifer made the decision to have chemotherapy – a plan specified for eight rounds at two-week intervals.
“I started chemotherapy in late July and completed it at the end of October. At the end of it, the pathology report that came back found a small amount of cancer remaining in my breast, but very minor,” Jennifer said. “They couldn’t find the lump anymore in my breast, and the tumor in my lymph nodes completely disappeared.”

While chemotherapy was a tiring process, Jennifer’s response was positive and meant that surgery with UT Physicians breast and endocrine surgeon Emily K. Robinson, MD, would be less extensive.
“Due to the BRCA2 mutation, we went forward with a double mastectomy to prevent the development of cancer in the future. Because the chemotherapy went so well in killing the tumor cells, it was only necessary to remove the previously positive lymph nodes and not a full dissection,” said Robinson, who is a professor in the Department of Surgery at McGovern Medical School at UTHealth Houston.
Jennifer’s double mastectomy was combined with a reconstructive plastic surgery procedure.
“Because we were able to save much of the skin and tissue that had been over the tumorous mass, it made the opportunity for immediate reconstruction even more promising,” Robinson said. “Jennifer was able to return home the same day, and she healed very well cosmetically.”
Jennifer was very highly pleased with the outcome, after all that she had experienced.
“Honestly, the results were beautiful. I was just so happy with it,” Jennifer said. “The surgeries performed were magic.”
Following the surgeries, Jennifer did a 30-day cycle of radiation treatment. Additionally, Jones prescribed a regimen of polymerase (PARP) inhibitors and additional hormonal therapy to reduce Jennifer’s estrogen levels. This novel strategy is part of some of the newest methods being used to treat BRCA-positive patients for both breast and ovarian cancers.
“Jennifer’s treatment embodied some of the most up-to-date treatments being offered for young women. By starting with chemotherapy prior to surgery, it allowed the opportunity for tailored surgical and radiation decisions,” Jones said. “Also, the incorporation of hormonal therapy to combat estrogen-positive cancers is showing results in reducing risks of it ever coming back and can be combined with other medicines, if necessary.”
In reflection, Jennifer is grateful for the treatment she received and feels empowered to share a message with others about her path to recovery and being proactive.
“I can’t say enough for Dr. Jones and Dr. Robinson. It was a godsend hearing another opinion, as I think it saved my life,” she said. “Through it all, I learned the power of being an advocate for yourself, and I encourage my friends to closely mind their personal health, performing self-exams and having regular screenings with their doctors. It’s about being strong as women and making each day count. Cancer is not the end of the world.”


