Angela Meshack has dedicated her life to education and advocacy. She earned Master and Doctor of Public Health degrees from UTHealth Houston School of Public Health, where she also launched her health career.
“I spent 14 years working in research at UTHealth Houston, part of it in cancer prevention,” said Meshack.
She went on to become a tenured professor at Texas Southern University. Just one year before her retirement, she felt something wasn’t right with her body.
“My primary care doctor said the pain and changes were related to my age,” she recalled. “I was told my symptoms were happening because I was getting older.”
But she knew her body and pushed to find answers.
A colonoscopy revealed a significant mass, and after meeting with several specialists, she learned it was likely an endometrial-related cancer.
“I was shocked, and I was angry,” she said. “I thought I had taken care of this.”
Endometriosis diagnosis
Throughout her adolescent and adult life, Meshack suffered intense pain and heavy bleeding during menstrual cycles.
“It was very difficult emotionally and physically,” she said.
At 28, she was diagnosed with endometriosis.
Endometriosis is a condition in which the endometrial cells that line the inside of the uterus grow outside the uterus.
Symptoms of endometriosis include pain and heavy bleeding during periods, and if untreated, the condition can lead to infertility. There is no known cause.
Treatment for endometriosis
Meshack spent 12 years searching for a solution.
“I tried all kinds of medical interventions, from birth control to laparoscopy to hormone suppression, but the endometriosis continued to come back,” she said. “It was impacting my quality of life.”
By age 40, she yielded to her gynecologist’s recommendation and underwent a hysterectomy.
“Going through early menopause was difficult,” she said. “At first, I was worried I’d feel like less of a woman, but over time, I came to accept it and appreciate it.”
The hysterectomy seemed to improve her quality of life, eliminating pain and heavy bleeding. After surgery, she began hormone replacement therapy to ease symptoms of early menopause, specifically hot flashes.
Life continued, and she excelled professionally, co-authoring more than 45 peer-reviewed articles in various public health journals and editing an autobiography.
But more than two decades later, the endometriosis returned, and this time, it was cancerous.
Endometriosis-related cancer
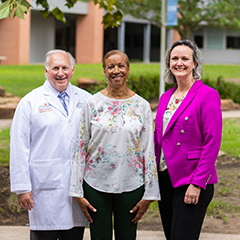
Meshack was referred to Joseph A. Lucci III, MD, a gynecologic oncologist, and Marianne V. Cusick, MD, a colorectal surgeon, both with UT Physicians.

“A biopsy found endometrial tissue was invading tissue in the colon, rectum, and vaginal tissue,” said Cusick.
Her doctors diagnosed Meshack with a rare endometrial cancer called Mullerian clear cell carcinoma.
She was shocked, confused, and disappointed. The condition that plagued her young adult life, stole fertility from her and forced her into early menopause had come back and was threatening her life.
Lucci estimates that less than 2% of women with endometriosis will develop cancer within an endometriosis implant.
“Endometrial cells have a tendency to invade other tissues, and over time, if exposed to estrogen, they can transform into a cancer,” explained Lucci, a professor and director of the Division of Gynecologic Oncology with McGovern Medical School at UTHealth Houston.
He says that doctors likely left residual amounts of the endometriosis behind during the hysterectomy, which is common because it is difficult to identify and remove all endometriosis implants during surgery.
“Those residual cells continued to grow and respond to hormones, just like the endometrial lining does,” he said.
Surgery and treatment
Lucci and Cusick recommended surgery, the most effective treatment for endometrial-related cancer.
The care team at UT Physicians worked swiftly, and Meshack underwent surgery within three months of her colonoscopy.
Using a minimally invasive robotic technique, Cusick and Lucci worked together to remove the cancerous portions of her colon, rectum, and vagina.
Recovery
The surgery was successful, and the hospital discharged Angela 48 hours later. Within three weeks, she was back to an active lifestyle.
“Recovery time from this type of surgery is typically short,” said Lucci. “You can get back to a normal, daily routine, minus strenuous activity or exercise, pretty quickly.”
Chemotherapy
Following surgery, Meshack underwent six rounds of chemotherapy over three months, which she tolerated well with minimal side effects.
Back to life
Less than a year after that colonoscopy, doctors declared Meshack cancer-free, and she celebrated with her family and friends. The surgery and chemotherapy did not adversely impact her organs, and she continues to live pain-free. She describes her quality of life post-surgery as “outstanding.”
“Being declared cancer-free was very exciting. I was relieved,” she said. “I felt like I could exhale.”
After a career devoted to research, advocacy, and teaching, she found the answers to her biggest challenge back where it all began – within UTHealth Houston.
“During a time when I really needed it, the university and my doctors were there for me. Dr. Lucci and Dr. Cusick were incredibly caring people who eased my fears, answered all my questions, and treated me with respect and compassion.”


