- UTHealth Houston Fetal Center
- Fetal Intervention for Congenital Diaphragmatic Hernia (CDH)
Fetal Intervention for Congenital Diaphragmatic Hernia (CDH)
The UTHealth Houston Fetal Center expertly manages pregnancies impacted by congenital diaphragmatic hernia (CDH) through a multidisciplinary approach. Our program brings together a comprehensive team of specialists in maternal-fetal medicine and fetal surgery, as well as pediatric subspecialists, to guide patients as they navigate this complex diagnosis. We recognize the distinct health concerns that women with CDH may encounter. Whether it involves obstetric care during pregnancy or managing gynecological and internal medicine issues, The Fetal Center provides personalized and comprehensive support to address their individual needs.
6410 Fannin St, Ste 210
Houston, TX 77030-3004
Fetal Surgery for CDH
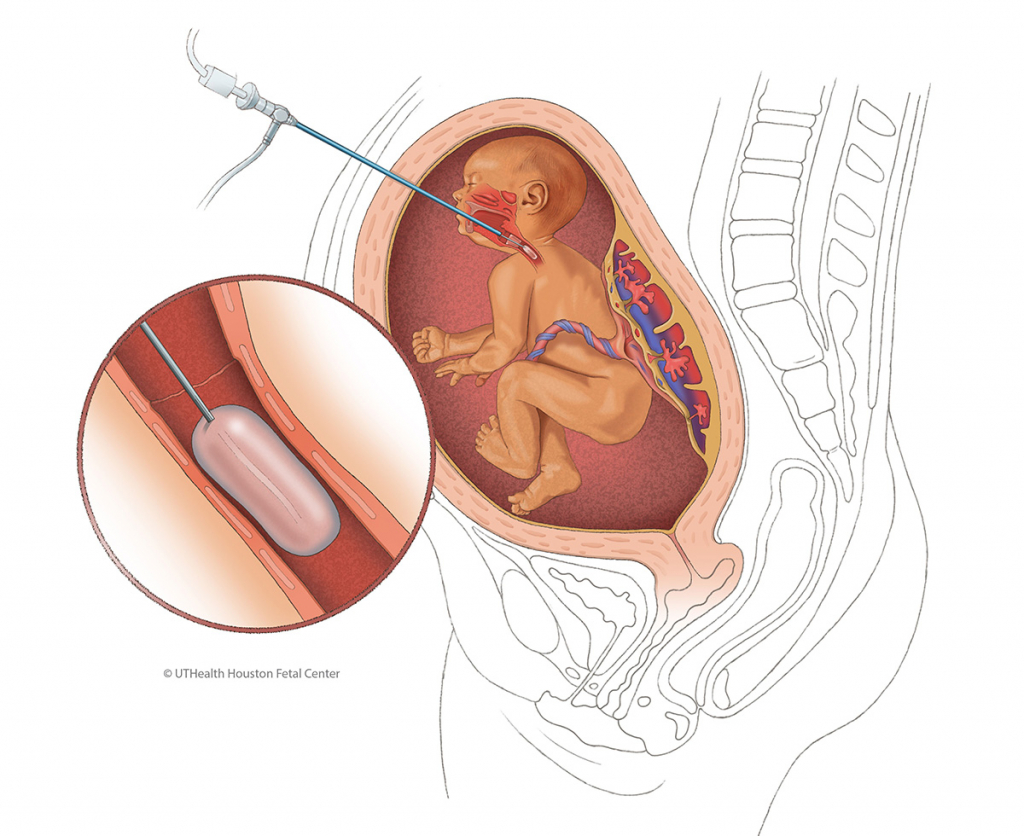
As leaders in the prenatal treatment of CDH through fetoscopic endoluminal tracheal occlusion (FETO), physicians at The Fetal Center actively participate in international research trials, offering the latest techniques for addressing severe CDH in-utero.
Although the goal is to repair the hole in the diaphragm after birth, the main concern for infants with CDH is the lack of mature lungs, heart malfunction, and abnormal blood vessels that carry blood from the heart to the lungs that develop in-utero. UTHealth Houston is one of the sites in the United States that has FDA approval to provide fetal surgery for CDH through FETO.
Mothers who qualify and decide to move forward with the in-utero FETO procedure will undergo a surgical procedure at approximately seven months into the pregnancy, during which a scope is used to place a tiny balloon in the baby’s trachea. Normally, the fetal lungs produce fluid, which escapes through the trachea and mouth into the amniotic sac. The balloon ensures that this fluid remains in the lungs, increasing pressure, which may stimulate lung growth. The balloon stays in place for five to seven weeks.
FETO is not appropriate for every CDH patient. We collaborate with families to discuss options and make the best, personalized decision for the unique circumstances of each patient.
What is CDH?
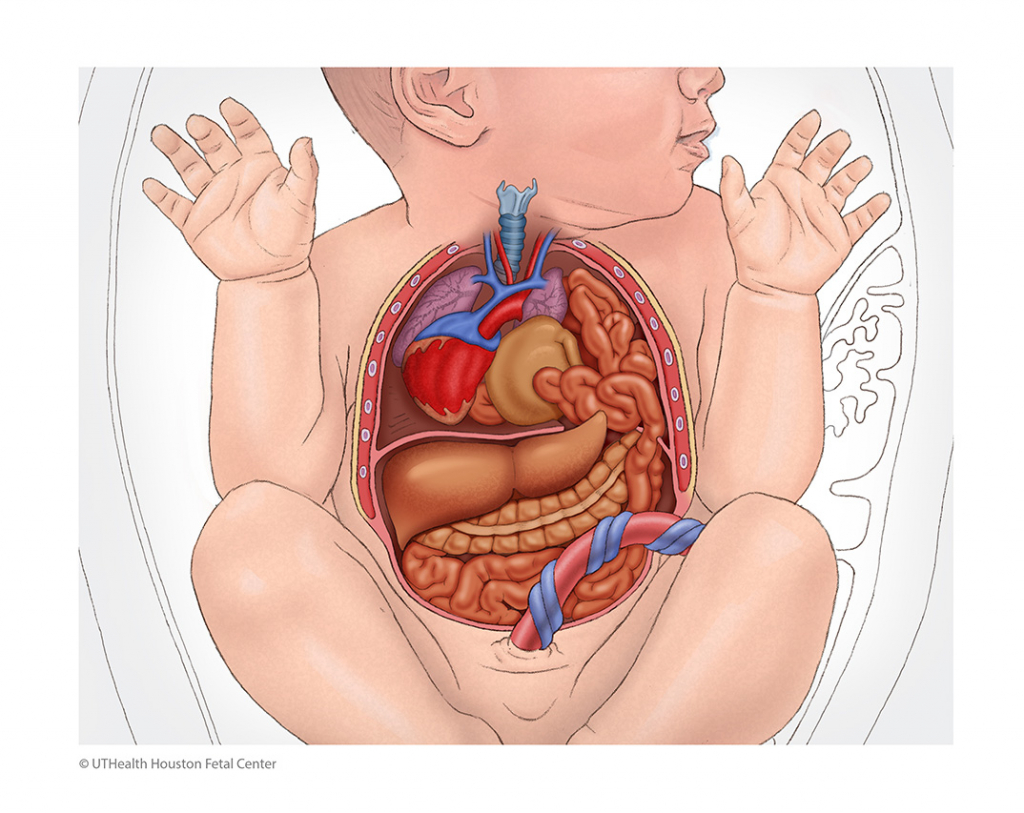
Congenital diaphragmatic hernia (CDH) is a hole in the diaphragm, a sheet of muscle separating the organs in the abdomen from those in the chest. Abnormal development of the diaphragm before birth causes the defect, which may range from a small hole to the complete absence of the diaphragm.
The hole, which may occur on either the right or left side, may allow abdominal organs – including the intestines, stomach, and liver – to move upward into the chest. When an organ pushes through the hole, it is called a hernia, which can compress the lungs during their critical development period. Babies born with smaller-than-normal lungs due to CDH may have difficulty breathing at birth. Some infants have other serious complications, including brain, heart, kidneys, and bowel developmental problems.
Physicians and researchers estimate that about 1 in every 2,500 to 3,000 live births is a baby with CDH. Most infants are diagnosed before or shortly after birth, although less severe cases may be identified later in life.
CDH can be a life-threatening condition if not treated by highly experienced, board-certified prenatal, neonatal, pediatric, and adult medical experts before and after birth. While optimized care throughout the CDH journey can significantly improve quality of life, every step, patient, and family is unique. Our comprehensive program at UTHealth Houston guides and supports families before and after their child is born.
CDH is usually discovered during the first anatomy scan at about 20 weeks of gestation when ultrasound shows abdominal organs located in the baby’s chest. Less severe cases may be discovered after birth.
Careful prenatal monitoring is essential to confirm the CDH diagnosis and monitor fetal development and growth. Your physicians may recommend additional tests, including fetal MRI and fetal echocardiogram, to determine the severity of the hernia and identify other problems. An amniocentesis also may be recommended to identify potential chromosomal abnormalities.
CDH can be life-threatening and should be treated by a highly experienced team of subspecialized physicians and nurses from maternal-fetal medicine, neonatology, critical care, pediatric surgery, pulmonology, and specialists who treat adult CDH patients.
- Complications and long-term health depend on the severity of the CDH.
- Even patients with mild CDH face the potential for short- and long-term consequences without appropriate care.
- Optimized care throughout the CDH treatment process and into adulthood can significantly improve quality of life.
Fortunately, the prognosis is improving. After evaluating each child and family, we provide a specific prognosis based on numerous factors.
- Care for patients of all ages, from prenatal (before birth) to neonatal (after birth) to pediatric (children) and into adult care
- One of the few fetal centers in North America offering fetal surgery for CDH through fetoscopic endoluminal tracheal occlusion (FETO)
- Continually advancing the expertise and infrastructure necessary to care for all patients with this diagnosis
- Identify and address common CDH challenges before they become life-threatening
- Advance CDH research through multicenter prenatal research studies and Congenital Diaphragmatic Hernia Study Group to help individuals of all ages with CDH
- Coordinate the scheduling of visits, obtaining/sharing imaging/labs, and leverage telemedicine when appropriate
- Help guide pregnant patients carrying a child with CDH and those who had CDH themselves with family planning/pregnancy support through The Fetal Center
Continuum of Care
With a collaborative and multidisciplinary team of maternal-fetal medicine, pediatric, and adult experts, we ensure seamless care from prenatal and infant stages through adulthood. Our facilities are under one roof, allowing us to address unique challenges at different life stages, with specialists in neonatology, pediatric surgery, thoracic surgery, pulmonology, adult general surgery, and OB/GYN working together for optimal patient outcomes.

