Aortic Disease
What is Aortic Disease?
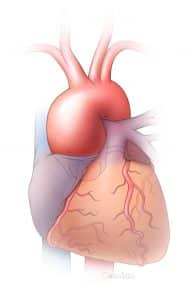
Aortic disease is broadly defined as conditions affecting the aorta, the main and largest artery in the human body that supplies oxygenated blood to all of the body’s vital organs. When the aorta becomes diseased or damaged, the entire body’s blood supply can be jeopardized and can quickly transform into a serious medical emergency.
What is the Aorta?
The aorta starts at the root of the heart, where the artery is connected to the heart by the aortic valve. It hooks like a candy cane down the spine, sending blood to the, brain, arms, spinal cord, visceral organs (intestines, liver, stomach), kidneys, and legs.

Aortic Aneurysm
An aortic aneurysm is a “ballooning” of the aorta that, if expanded far enough, can potentially rupture. An aortic aneurysm can occur in either the chest region, commonly called a thoracic aneurysm, or the abdomen region, often referred to as an abdominal aortic aneurysm (AAA).
Aortic Dissection
Aortic dissection occurs when the middle layer of the aortic wall splits creating a “false” channel for blood flow. This dissecting process weakens the aortic wall making it more prone to rupture. When rupture occurs, survival is often less than 10%. Aortic dissection can also lead to obstruction of any of the branches of the aorta and ultimate organ death. Although many risk factors for aortic aneurysms have been identified, the exact cause remains unknown.
Thoracoabdominal Aortic Aneurysm
Thoracoabdominal Aortic Aneurysm (TAAA) is an enlargement or ballooning in the aorta, the main artery in the body that supplies blood to the rest of the body. TAAA occurs in the thoracic aorta, the upper section of the aorta close to the heart and chest, and extends into abdominal aorta. If left untreated, the aneurysm can rupture, leading to severe pain and lethal internal bleeding.
Symptoms, Causes, Prevention & Early Detection of Aortic Disease
Symptoms of Aortic Disease
Sudden stabbing, radiating pain, fainting, difficulty breathing, and sometimes sudden weakness on one side of the body could suggest an aortic event. Clammy skin, nausea and vomiting, or even shock are also common accompanying symptoms. Aortic disease can also mirror symptoms of a heart attack, such as chest pain or jaw pain. The aorta spans from above the heart all the way down to below the navel, so symptoms of pain can occur at any place along the torso.
Causes of Aortic Disease
Genetics and family history of aortic disease contribute significantly to the risk of developing an aortic aneurysm or dissection. In addition to genetic factors and age, people who experience the conditions below have an increased risk of aortic disease.
- High blood pressure – the increased force of blood can weaken the artery walls
- Marfan syndrome or other genetic conditions – can cause problems with the body’s ability to make healthy connective tissue
- High cholesterol or atherosclerosis – a buildup of plaque may increase inflammation in and around the aorta and other blood vessels
- Inflamed arteries: – the body’s blood vessels can become inflamed due to trauma from car accidents or certain diseases like vasculitis
- Smoking – people with a history of smoking are three to five times more likely to develop an aortic aneurysm
Prevention & Early Detection of Aortic Disease
The U.S. Preventive Services Task Force, an independent, volunteer panel of national experts in disease prevention and evidence-based medicine, recommends that men aged 65–75 years who have ever smoked, be screened for abdominal aortic aneurysms, even if they have no symptoms. Screenings are done by a noninvasive vascular ultrasound and is completely covered by Medicare for qualifying individuals.
People living with aortic disease, or who have a family history of aortic disease should be proactive with their health and report any symptoms immediately. It is important to get regular check-ups, and always take care of your overall heart health.
Genetics
Hereditary Aortic and Vascular Disease
Genetic triggers play an important role in causing thoracic aortic aneurysms, aortic dissections, and other related vascular diseases. Identifying the underlying genetic cause of aortic and vascular disease through genetic testing enables that person’s healthcare team to develop a personalized medical management plan. This information also helps identify family members who are at risk for developing an aneurysm or dissection in the future so their healthcare providers can proactively implement a screening and management plan to prevent the life-threatening complications from aortic dissections.
Signs of genetically-triggered aortic and vascular disease are not always obvious, and many individuals diagnosed with aneurysms or dissections do not know that they have a genetic predisposition. Individuals and with a personal or family history of aortic disease should consider genetic counseling and testing if they have any of the following: 1) Family history of aneurysms, dissections, and early sudden deaths 2) An aneurysm or dissection of the aorta or other artery diagnosed at an early age, typically before 60 years, or 3) Physical signs of a genetic syndrome such as Marfan syndrome, Loey-Dietz syndrome or Vascular Ehlers-Danlos syndrome. However, many people with heritable aortic and vascular disease (HTAD) have no outward physical signs of a genetic syndrome. Genetic testing and counseling can help clarify risk.
UTHealth Houston has a multidisciplinary aortic and vascular genetics team of experts dedicated to evaluating and caring for individuals with HTAD. Our core team includes providers from cardiothoracic and vascular surgery, cardiology, and medical genetics. Many people with HTAD have other risk factors for aortic disease such as high blood pressure (hypertension) or a bicuspid aortic valve (BAV), requiring a multidisciplinary team for comprehensive care. To request an appointment in the multidisciplinary aortic and vascular disease clinic (MAVC), please contact us at cvgenetics@uth.tmc.edu or 713-500-6715.
The John Ritter Research Program in Aortic and Vascular Disease, directed by Dr. Dianna Milewicz at UTHealth Houston, is focused on identifying genetic and other risk factors that contribute to thoracic aortic aneurysms and dissections. The goal of this research is to better understand these risk factors to improve diagnosis and treatment strategies and ultimately, prevent aortic dissections. For more information about this research, please email JRRP.research@uth.tmc.edu.
Treatment & Management
If identified early, aortic disease can be managed medically with frequent monitoring, medication and adjustments in lifestyle.
Surgical treatment options include minimally invasive procedures (referred to as endovascular repair), or open repair. Surgical treatment is intended to reconstruct or replace the affected area of the aorta. Such surgical procedures include the placement of a stent or stent-graft, which can be placed through open repair, endovascular repair (minimally invasive), or a hybrid approach combining the two. The most common treatment modalities are open repair of ascending aorta for type A dissection, and thoracic endovascular aortic repair (TEVAR) for type B dissection.
Open Abdominal Aortic Aneurysm Repair (AAA)
During this procedure, the abdominal segment of the aorta is replaced with a prosthetic tube graft through an open incision. This procedure requires general anesthesia. The hospitalization period is 5-7 days and full recovery can take a few weeks. The Department’s outcomes are among the best in the country.
Endovascular Abdominal Aneurysm Repair (EVAR)
The minimally invasive endovascular abdominal aneurysm repair (EVAR) procedure involves making small incisions in the groin and threading catheter tubes through the femoral arteries and into the aorta. A fabric-covered metal stent is introduced through the artery and fixed in place, relieving pressure on the artery to prevent rupture. Patients remain conscious under local anesthesia during the procedure. Patients who undergo EVAR have lower morbidity rates and shorter recovery times and can usually resume normal activity within a few days after surgery.
Thoracic Endovascular Aortic Repair (TEVAR)
A minimally invasive alternative to open surgical repair of diseases of the thoracic aorta, TEVAR is most commonly used to correct thoracic aneurysmal disease. Using the TEVAR procedure, the vascular surgeon inserts an endograft (fabric covered stent) into the aneurysm as a replacement for the diseased segment of the aorta. Patients benefit from reduced mortality and morbidity, shorter hospitalizations and more rapid recovery.

